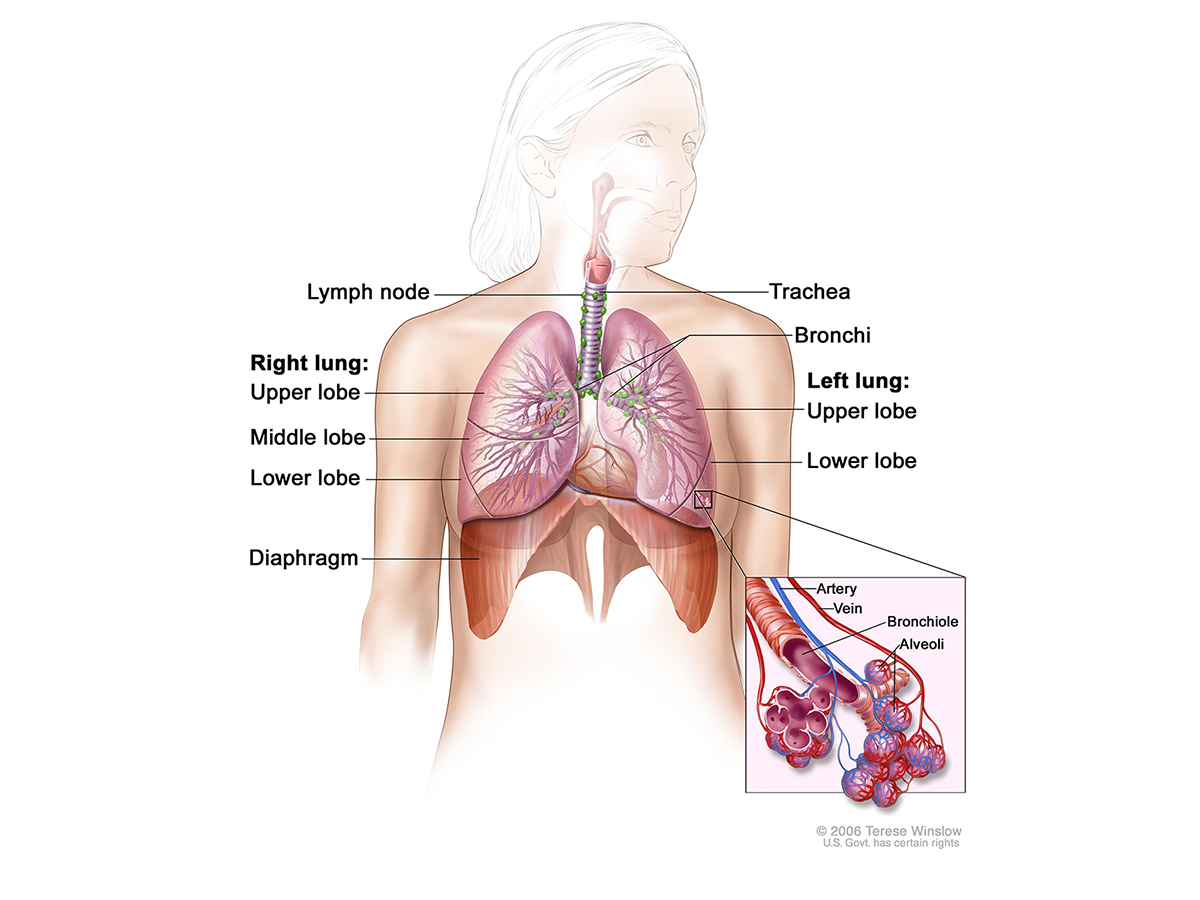
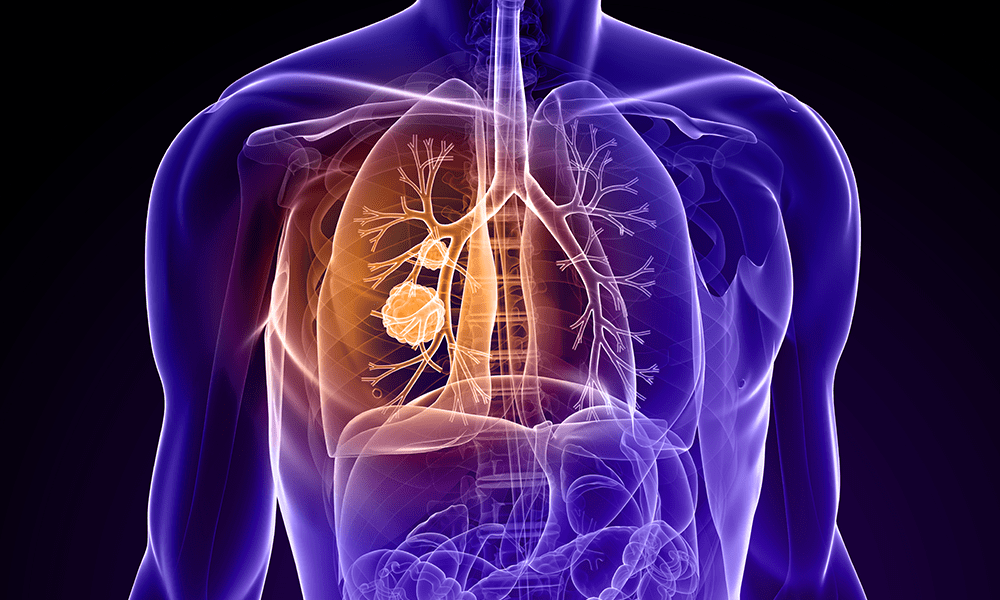
Thoracic cancer refers to any cancer located in the organs, glands, or structures of your thoracic cavity, or chest. This includes well-known cancers such as lung cancer (currently the second-most common cancer among both men and women) and esophageal cancer, as well as less common cancers such as thymus cancer and pleural cancer.
The oncology professionals at Dignity Health are here to support you through your journey with thoracic cancer. Find a Doctor today to set up a personalized treatment plan.
The most significant risk factor for thoracic cancer is smoking. Almost all lung cancers occur in people who previously or currently smoke. Small-cell lung cancer, in particular, rarely occurs in people who haven’t smoked.
The more time you spend smoking, and the more cigarettes you smoke, the higher your risk. Being around other people who smoke also increases your risk. This “second-hand” smoke causes thousands of cases of thoracic cancer every year.
Other common risk factors include:
Thoracic cancer symptoms vary based on the specific cancer type and the tissue it affects. In the early stages, there are often no symptoms, and as a result, thoracic cancer is harder to diagnose until it is at an advanced stage.
When symptoms do occur, they may include:
If you have several risk factors for thoracic cancer, such as family history, workplace exposures, or history of smoking, your doctor may recommend preventive screenings even if you do not have symptoms. Screening checks typically involve chest x-rays or other imaging tests to look for any abnormalities.
Other cases are diagnosed after symptoms. Some standard diagnostic tests include:
Thoracic cancer treatment options vary according to the type of cancer you have. Surgery is a standard treatment. Your doctor may also recommend the following treatments:
Some people develop the disease even if they do not have any known risk factors. Talk to your doctor to learn more about personalized treatment for thoracic cancer.